On Wednesday and Thursday of this past week, Rick Fulton of the Gettysburg Times, wrote reported that WellSpan hospital system in Central Pennsylvania will no longer support or offer to provide blood testing for Court use of Blood Alcohol Content testing (BAC). The BAC testing, of course, is so important in a DUI prosecution and is one of the fundamental pieces of, and oftentimes the only, evidence against a citizen among us who has been accused of a DUI Rick Fulton wrote a great article. You can access it in full here “Hospital explains ban on DUI tests”.
It presents two main issues as to why the Hospital system will no longer offer or support BAC testing. I am proud to say that our firm, The McShane Firm, LLC has been successfully litigating both aspects in Pennsylvania. In fact, to our knowledge no other attorney or firm has advanced these types of defenses in Central Pennsylvania and likely not in the entire Commonwealth of Pennsylvania.
In his article reporter Rick Fulton wrote:
William Lavery, manager, WellSpan Office of Health Public Relations & Communication at Gettysburg Hospital, confirmed Wednesday that the testing service was being discontinued at the hospital, but that the facility will continue to draw the blood.
[William] Lavery, manager, WellSpan Office of Health Public Relations & Communication at Gettysburg Hospital] stated there were two fundamental reasons for the discontinuation of the service, the first concerning accreditation of the hospital’s laboratory and the second relating to increased demands on the laboratory.
Regarding accreditation, he said, “In our case, the hospital laboratory is unable to meet a new testing regulation introduced by the College of American Pathologists. They generate standards and they are our primary accreditation agency.”
“If we were to lose accreditation by not adhering to their regulations, we’d really jeopardize the lab’s primary role of providing health care to our patients,” Lavery said.
In addition, the legal system, particularly DUI defense attorneys, are demanding more and more from laboratories that conduct BAC testing.
This is causing an increasing drain on the hospital’s resources.
“It’s (legal demands) becoming an increasing impact on our lab resources…trying to meet the legal requirements that these cases (generate),” he said.
“More and more,” Lavery stated, DUI defense attorneys subject the hospital lab’s to strenuous (expectations), which include responding to subpoenas that go beyond the hospital’s ability to respond to them.
“Attorneys are mandating that a clinical (hospital) lab be able to demonstrate forensic abilities, to respond to documents, provide staff competency documentation…those are things a forensic lab is more equipped to handle,” he stated.
The load and responsibility has caused an “increased demand on our resources…A clinical (hospital) lab may not be able to operate (the same level of service) as a forensic lab,” Lavery stated, pointing out that what is being asked of the hospital’s clinical laboratory are things that a forensic lab deals with routinely.
…
The majority of the hospitals in the area (south central Pa.), he noted, have already ceased DUI testing, according to the communications manager. “A lot of area hospitals made that decision a couple of years ago.”
I have blogged about this first issue in “Piece of Paper Says Your Guilty”. It outlines the recent United States Supreme Court decision of Melendez-Diaz and its import.
The Real Problem
Now I want to complete the thought of the article and blog about the absolute consensus of the scientific community that hospital blood testing is not forensically acceptable. I will try to explain why as briefly as I can. For over five (5) years, I have personally been leading the fight in Pennsylvania in this area of medicolegal litigation pushing the science or really the lack of forensic reliability of hospital blood BAC testing.
First some background….
In the Commonwealth of Pennsylvania, there are various degrees of prohibited BAC levels, called per se levels. They are 0.08, 0.10 and 0.16 with enhanced penalties depending upon what your blood level is. These per se levels are measured as grams percent AND MUST BE expressions of whole blood. A conviction on a per se offense cannot be based upon plasma or serum. The expression of the BAC must be to whole blood and whole blood only.
So, we begin at the beginning, shouldn’t we?
Are hospital blood tests truly whole blood tests?
As shocking as it is to most people, the real answer is NO.
There is but one analytical device that performs a whole blood analysis, it is called a gas chromatograph. It has a detector to allow for quantification which is usually a Flame Ionization Detector. Using a mass spectrometer is the best way of conclusively confirming the analysis, but it is not often used.
So what are they doing?
The hospital based blood test performed at the hospital is scientifically referred to as a plasma enzymatic indirect test based on spectrophotometry (colormetic response) of treated de-proteinzed vortexed, centrifuged aspirated supernate of the original whole blood specimen.
Wow what the heck does that mean? Don’t worry keep reading and I promise it will all make sense to you.
We will shorten all of this up and simply refer to it as “hospital blood” or “hospital blood testing”.
Ok. So let’s take it step by step.
PROBLEM 1:
An “enzymatic indirect test” means that we are not testing how much ETOH (drinking alcohol or Ethyl Alcohol) is in the whole blood. Instead what we are testing is an indirect measure. We use a known enzyme (NAD+) amount and hope that it will react to ETOH and create a quantifiable result as the two interact resulting in Acetaldehyde+NADH+H+
So chemically, it looks like this….
Ethyl Alcohol+ NAD+ —-> Acetaldehyde+NADH+H+
Instead it is measuring the reaction difference to an enzyme at a specific wavelength. Hospital analysis is by enzyme assay. An enzyme is added to the totally prepared sample. That enzyme (NAD) reacts in the presence of alcohol (and other things) and forms another enzyme (NADH). The amount of NADH is then measured (as relative to the NAD remaining) to determine the amount of alcohol in the sample.
Still don’t follow? Don’t worry, I follow through on all of my promises keep reading. I will make it clear.

Ok it’s really simple if we relate it to something we know—the good old bathroom scale.
I want you to suppose that you want to know how much your 6 year old daughter weighs. There are basically two (2) ways: a direct way and an indirect way.
What would make the most sense and is the most accurate is to take out your bathroom scale and put your daughter on it and voila, we have the weight. This would be like using a Gas Chromatograph. It is a direct measure of the weight of your daughter.
Now, let’s think about another way to try to get at her weight. I suppose you could step on the scale and see how much you weigh (a known), get off the scale and then have your 6 year old daughter hop on your back piggyback style and then both you and her on your back step on the scale having seen what your combined weight is. You both get off. You would then take your combined weight and subtract it from your known weight that you got on the first measurement and voila, you might have her weight.
What happens next? Your spouse who watched the whole escapade looks at you with a puzzled look and says you are silly and she doesn’t understand why you did it this indirect way when the direct way would be easier and more accurate. This is exactly like hospital blood.
Makes sense now, right? Good.
In conclusion, indirect measurements are never forensically or scientifically acceptable when there is a direct method available. That is the first reason why hospital blood is forensically and scientifically unacceptable.
PROBLEM 2:
Issue number two is the type of analytical measuring device used. It is based on spectrophotometry (a colormetic response). Spectrometry is grossly over simplified as this. Spectrophotometry involves the use of a spectrophotometer. A spectrophotometer is a photometer (a device for measuring light intensity) that can measure intensity as a function of the color (or more specifically the wavelength) of light. Important features of spectrophotometers are spectral bandwidth and linear range of absorption measurement. It is rooted in Beer’s Law.
In short, the sequence of events in a spectrophotometer is as follows:
- The light source shines into a monochromator.
- A particular output wavelength is selected and beamed at the sample.
- The sample absorbs light.
We use an energy source such as a light, and a detector (specifically a photo detector) on the other end of sample chamber. Then we run the sample, or analyte, in-between the energy source and the photo detector. If the analyte is not present, it is smooth sailing as the energy emitted by the energy source should not be impacted (i.e., no loss of signal energy-it remains at the same strength). If there is analyte present, then it will interfere with the energy emitted by the energy source. The photo detector detects less energy. A comparison is made between what we would expect versus what we got as measured by the photodetector.
Colormetric means that there is a color response (lighter or darker in this case) that depends upon the concentration of the analyte.
Wow? What does that mean?
Here are good pictures that show what I was conveying.
Think of taking a laser pointer and trying to shine it through a glass of clear water versus a glass of Kool Aid. The laser pointer will mostly go through the clear water with little loss of signal, but the Kool Aid experiment will result in much less signal going through. It’s that simple.
PROBLEM 3:
The third issue concerns the limitation of the technology itself. As mentioned above, the machine is based upon spctrophotometry and is a colormetric response. As such we need something that is basically pure and clear. Otherwise, if it is dark and dirty, then the response is not utterly remarkable. In other words, you cannot tell. What is dirty and darker than blood?
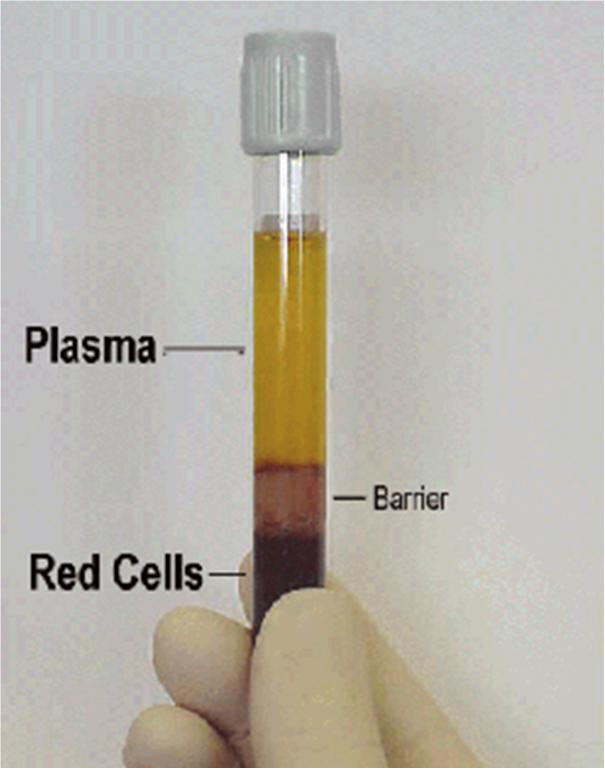
Blood is a viscoelastic complex matrix full of a lot of stuff. Hence, plasma is used. Whole blood is defined as blood from which none of the elements have been removed. Plasma is defined as the fluid portion of the blood in which particular components are suspended. The components that are suspended consist of red corpuscles, white corpuscles and platelets. Whole blood and plasma look very different as one can see below.

So to clean it up, and transform it into plasma, they have to do the following. They have to strip the protein from it. This is done by adding a de-proteinizing agent such as Trichloroacetic Acid (TCA). TCA will bond with the protein and after centrifuging, it will become solid and a noticeable pellet will form at the bottom.
The blood is further transformed through the centrifuging process. Just like anything that is centrifuged, the heavy parts go to the bottom and the lighter parts are separated to the top. This is called the supernate (the top stuff) and the precipitate (the bottom stuff) division. With blood, heavy parts such as the blood’s red blood cells and the pellet from the TCA reaction are at the bottom. The plasma and the alcohol (if there is any) are at the top because they are lighter.
Next the top part is removed by pipetting. This is called aspirating the supernate. [as an aside, one hospital lab surprisingly doesn’t use pipettes to get an accurate amount, but rather simply pours the supernate into a testing cup]. The aspirated supernate then makes its way into the analytical device.
Now if you are paying attention, you might be asking yourself “Hey? What happens to all of the rest of the specimen?” The answer is that it gets thrown out. It is never analyzed.
PROBLEM 4:
This is the perfect lead into the fourth issue as to why hospital blood is forensically unacceptable. It has to do with the legal requirements to sustain a conviction. As mentioned above, in the Commonwealth of Pennsylvania, there are various degrees of prohibited BAC levels, called per se levels. They are 0.08, 0.10 and 0.16 with enhanced penalties depending upon what your blood level is. These per se levels are measured as grams percent AND MUST BE expressions of whole blood. A conviction on a per se offense cannot be based upon plasma or serum. The expression of the BAC must be to whole blood and whole blood only.
So what do they try to do?
So in typical lawyer fashion, we try to force the round peg into the square whole and force a “conversion” factor that is supposed to adjust or convert the raw number for that big legal problem.
Sounds good in theory if you don’t mind the indirectness, but here is the dirty little secret. The scientific community cannot agree on what this all important number should be.
First, there is absolutely no consensus in the scientific community as to the proper conversion factor. There is no number. Therefore, as there is no scientific agreement, then no number should be used by the Courts. It is a basic Daubert/Frye matter. The government as the proponent of the evidence has the burden to prove it is reliable and based on sound science. The very fact that there are studies that conclude that there is overstatement of plasma to whole blood as low as 1.10 overstatement to as high was 1.59 make it so. That is a 69% swing. Come on! IN fact, it is now fairly well-settled that the relationship is nonlinear, which means that any conversion factor employed is letter better than a wild guess with no data to support it. The first to publish with data that there relationship is nonlinear was Barnhill, Herbert, Wells in their peer-reviewed study entitled “Comparison of Hospital Laboratory Serum Alcohol Levels Obtained by an Enzymatic Method with Whole Blood Levels Forensically Determined by Gas Chromatography.”
The conversion factor depends on hematocrit (packed cell volume) entirely (well almost entirely, but for the sake of brevity it is the most important part). Serum or plasma (almost-one article had a statistical artifact) always over estimates BAC. Plasma actually much more so.
PROBLEM 5:
The fifth issue has to do with the specificity. In order for a measuring device to be acceptable it has to measure only what it intends to measure specifically to the exclusion of everything else.
What does that mean?
If you went to Home Depot and bought a tape measure, but when you got it out of the box, it clearly was mislabeled in that it looks like a ruler, but you unspool it and it turns out to have no markings on it, and it turns out to have a thermometer in the middle of the spool. Boy that is a problem, isn’t it? They are both measuring devices: one for distance, the other for temperature. But the crappy tape measure that is really a thermometer is not a specific measuring device as to distance at all.
So here is a fundamental flaw as to hospital blood. It also is NOT specific to ETOH to the exclusion of all other matters. So, it is not direct and not specific.
Wow!
One of the well know problems is the use of IV administered ringers lactate. Some of our clients were at the hospital due to injury. If so, we would want to look for ringers lactate or any sort of ringers solution application being used OR if there had been any sort of significant trauma as that will release lactate as well.

A little history…Ringer’s saline solution was invented by Sydney Ringer, a British physiologist. The solution was further modified by Alexis Hartmann for the purpose of treating acidosis in children. Hartmann modified the solution by adding lactate, which mitigates changes in pH by acting as a buffer for acid. Thus the solution became known as ‘Lactated Ringer’s Solution’ and later, ‘Hartmann’s solution’ Lactated Ringer’s Solution is often used for fluid resuscitation after blood loss due to trauma, surgery, or a burn injury. Previously, it was used to induce urine output in patients with renal failure. Lactated Ringer’s Solution is used because the byproducts of lactate metabolism in the liver counteract acidosis, which is a chemical imbalance that occurs with acute fluid loss or renal failure.
The intravenous dose of Lactated Ringer’s Solution is usually calculated by estimated fluid loss and presumed fluid deficit. For fluid resuscitation the usual rate of administration is 20 to 30 ml/kg body weight/hour. Lactated Ringer’s Solution is not suitable for maintenance therapy because the sodium content (130 mEq/L) is considered too high, particularly for children, whereas the potassium content (4 mEq/L) is too low, in view of electrolyte daily requirement.
Why is this so important?
You have to understand that in a trauma situation, they don’t care about the legal ETOH. They care about keeping someone alive and not allowing them to go into shock. So, oftentimes they will put IV’s into each arm and infuse (i.e., squeeze the IV bag really hard and rapidly) to get into the veins as soon as possible. If they take the legal ETOH sample on the same arm, then they have really really large issues. It is an electrolyte replenishment therapy (i.e., fluid resuscitation). It invites havoc into the BAC determination and process.
The effect of ringers on a hospital blood test has to do with the manner of hospital analysis not the fact that the hospital test is a plasma test. As explained above, hospital analysis is by enzyme assay. An enzyme is added to the plasma sample when it is within the machine. That enzyme (NAD) reacts in the presence of alcohol and forms another enzyme (NADH). The amount of NADH is then measured (relative to the NAD remaining) to really indirectly determine the amount of alcohol in the sample.
So, the problem lies in the contents of the ringers lactate. The lactate reacts with LDH to form pyvurate. During this process additional NAD is converted to NADH, giving a false high alcohol result. In fact, it can give a positive alcohol reading where no alcohol is present. It is just frankly impossible to tell the true endogenous ETOH result.
The machine is totally blind to what is due to Ringer’s Lactate and what is due to a person drinking.Stated differently, the machine cannot tell the difference between ETOH created by this process and ETOH actually consumed by the person. All it sees is more NADH. Hence, it is not specific.
They can test for lactate levels but they never do.
Ringers lactate is not the only source of lactate, trauma (soft tissue or bone) also releases lactate. Lactic acid build up on a well-trained athlete can also interfere. Finally, shockingly in and of itself, TCA itself creates lactate! Remember TCA that was added to the sample itself as we described above.
PROBLEM 6:
The final issue has to do with the general scientific and legal communities’ view of hospital blood testing. Most of Europe, Asia and Australia abandoned hospital blood testing as a legitimate method of analysis for forensic purposes and bans them entirely from the Courtroom. This was done many, many years ago.
THERE ARE MORE REASONS
These and many more well-known problems have been well documented in the scientific community for decades.
There are actually a lot more than six (6) reasons why hospital blood is never forensically acceptable including, but not limited to: (a) the lack of meaningful detailed chain of custody for the tested specimen and all of the accompanying component materials making up the system of the test, (b) the lack of suitable criteria for preventive maintenance, (c) lack of or insufficient schedule of calibration both internal and external, (d) the lack of full documentation of or even the non-use of a third party vendor calibrators and blanks that are either traceable to NIST or USP grade materials, (e) the lack of true meaningful and independent blind proficiency testing of the technologist (the person who runs the sample), (f) the re-use of consumables such as the specimen prep cups and the TCA containers, and yes, even pipette tips without an acceptable Standard Operating Procedure that will insure cleanliness of the items reused, (g) the manufacturer of the machine’s own admonition that the machine is not intended to be used for forensic testing and so on and on and on.
Credit where credit is due….
I would be remiss if I did not commend WellSpan Hospital systems for acknowledging these important issues. I am told that this trend of recognizing the forensic unacceptability of hospital blood testing has continued with several other hospitals also similarly conceding the issue throughout Pennsylvania. I thank WellSpan for acknowledging and pledging to discontinue the unacceptable forensic practice of hospital blood testing.
So, it begs a question, doesn’t it?
We have been allowing hospital blood testing go on for decades with thousands upon thousands of convictions as a result. Not just here in the Commonwealth of Pennsylvania, but elsewhere in the United States.
Is there anything to be done for those who have been falsely convicted based upon forensically unacceptable science?
We did this with lead bullet analysis, DNA exonerations and other now abandoned quasi-forensic sciences, what will be done?
Or sadly is this yet another example of how there are another set of Rules that apply to DUI cases?
I also need to give a big thank you to the National College for DUI Defense, Inc. where I was exposed to these issues for me to latter develop. What a great group of scientist-lawyers who live the College’s motto: “Justice Through Knowledge”. Also an equally big thank you to various experts that have helped me through the years in developing my scientific and technical knowledge in this area. In no particular order they are: Dr. Joseph Citron, Dr. Thomas Brettell, Dr. Stephen Rose, Dr. Al Staubus, Dr. A. Wayne Jones, Wanda Marley and Janine Arvisu.
In closing, I offer this. As it seems likely that hospital blood will cease in the MidState in short time. If any attorney outside of Pennsylvania would like to mount well-developed Frye/Daubert challenges to hospital blood testing as we have done here, I am willing to help you free of charge. Heck, I will even conduct the cross and directs of the experts if you let me. I will pay my own way to the hearing. This is how important this issue is to me. Just contact me.
You can see my qualifications and experience at avvo.com
You can follow me on Twitter or Facebook or Linkedin.
[A special thank you to Josh D. Lee, Esquire of Oklahoma for helping to edit this work]
-Justin J. McShane, Esquire, Pennsylvania DUI Attorney
I am the highest rated DUI Attorney in PA as Rated by Avvo.com
You can follow me on Twitter , Facebook or Linkedin.
Evan Levow says:
I’ve said it before, I will say it a million times: Justin McShane is a genius. We are incredibly lucky to have him fighting for individual’s rights.
Gregory Oberhauser says:
Justin, great write up, direct versus indirect measurements is the key. thanks, Greg
Thomas Fike says:
So, if this has been known for decades why do they keep doing it? Doesn’t seem right.
Josh says:
It looks like Pennsylvania’s finest have been cutting corners once again. The need to find a proper way to prosecute DUI cases or risk endangering everyone.
Janina says:
Heya! It seems as though we both have a passion for the same thing.
Your blog, “WellSpan is to be commended, but why people who have been convicted for decades of a DUI should be upset | Pennsylvania DUI Blog” and mine
are very similar. Have you ever thought of authoring a guest article for a related blog?
It is sure to help gain publicity to your
blog (my site recieves a lot of traffic). If you’re interested, contact me at: janina_costa@gmail.com. Appreciate it